Well, it's a couple of days past Christmas, but I wanted to post anyway. This post is partially inspired by the Christmas Eve service, but I couldn't write it until now!
I celebrate Christmas, as the birth of Jesus of Nazareth. The Christmas story has always captivated me.
Even as a child, I could picture being heavy with child and wandering the streets with nowhere to stay, frightened and tired. I can imagine finding a cold, drafty barn - and can barely imagine giving birth, unassisted, in the hay. A young first-time and unmarried mother, with her fiance who may or may not (to the world) be the father of the baby, horses, cows and sheep as her midwives - no epidural or hospital delivery room here! When she delivered safely and finally held her baby boy in her arms, I imagine she looked into his newborn eyes and saw the face of God.
I know how she felt. I felt it, 9 months ago, when I first looked into my son's eyes. Holding a baby is like holding a piece of God.
Babies are magic. No matter your faith, there is something truly spiritual about holding a newborn child - yours or someone else's. You hold them and wonder where the soul inside came from, because clearly it is not far flung from that place. Everything else stops; all the worry, the fear, the "hustle and bustle." For the moments that precious soul curls up on your body, you would give anything to protect them from harm. You understand the meaning of "precious" and "priceless." Whenever I doubt the existence of something greater, I hold a newborn in my arms and I know, by some definition (even if not my own), He is real.
Christmas is celebrated at the winter Solstice, although research indicates that Jesus of Nazereth was likely born around September. As the early Christian church was encountering pagan nations, those people would not (could not) give up the celebration of this time each year, when the darkest nights finally give way to light and hope. What could be more hopeful than birth? So, the return of the Sun became the birth of the Son, the arrival of light into a dark world.
As we finish up our Christmas season, I hope you can hold a piece of Christmas in your arms. My hope for this year is that every child that enters this world be treated with love, as the magnificent gift that they are. I pray that we will all work to give those beautiful, freshly-delivered souls a world worthy of their innocence. If you are Christian, when you're holding that precious child in your arms, imagine the gift that God gave the world, if He sent His only son to us, to be our light through dark nights.
For every night, a child is born, every night a child is given. Every night is a Holy Night.
Merry Christmas, everyone.
Monday, December 27, 2010
Tuesday, December 21, 2010
Necesareans
Note: if you are planning a natural birth, especially with hypnosis, don't read this without your "Bubble of Peace" on Mega-Force-Field-Strength. If you are planning a peaceful, wonderful, pleasant and awesome birth and you want to visualize only wonderful happy things, click here for my favorite water birth video.
If you'd like to learn about real medical reasons for c-sections so you can potentially help avoid an unnecessary one, please proceed.
You've been warned. Bubble up?
Necesareans
The current US c-section rate is somewhere between 33 and 38% of all deliveries. The World Health Organization states that no region in the world should have a rate greater than 10-15%. If the WHO is correct, that means that 54%-73% of all American cesarean deliveries are unnecessary. Average the numbers out, and that means that 2 out of every 3 c-sections performed in the USA may be unnecessary. Let’s play with some pretend, averaged and hypothetical numbers.
 |
| The 2010 rate is estimated at 33.9%. |
100 laboring women. 33 have c-sections. 22 women had surgery they may have been able to avoid.
Now here’s the twist. 11 of them did need c-sections. There are valid medical reasons for c-sections. Women used to die in labor, far more often than they do today. Babies used to die in horrific numbers during childbirth, and the c-section is an amazing medical advance, a relatively “safe-ish” surgery that can and does save lives. Before the advent of the c-section, labor and delivery were leading causes of death for young women and babies. Since 1980 (and not on this chart), the number of maternal deaths is rising again, and many say it is because of the overuse of the cesarean section.
 |
| Maternal deaths per 100,000, 1880-1980 |
How do you know which one you are? Is your birth a real emergency, one of the 11, or one of the 22 that might have been avoided and could be putting you and your baby at needless risk? Your doctor will always tell you that you’re one of the 11, unless you have an elective surgery (very rare – despite the hype, less than 0.5% of c-sections are truly elective, with zero “medical” reasoning provided). Your doctor will always say that you had a c-section because it was necessary.
So, you’re in labor, or close to it. Things aren’t going according to plan. Your doctor wants to do a c-section, and they’ve been to medical school. You haven’t. How do you keep from being part of the 22? How do you know if you’re one of the 11? Ultimately, you have to trust your care provider, which is why selecting one is so very important. You also have to do everything you can to reduce your risk of running into a real medical reason (avoiding interventions unless they are medically necessary).
Below is a list of medical indications for cesarean section, with details. Knowledge is power, right?
As always, please note: I am not a doctor. I have not gone to medical school. I have never performed a c-section. I am not an expert. I am a mommy who likes to write stuff and post it on the internet. Please do not take anything I write as medical advice, but as information and opinion. Inform yourself, do your own research, and talk to your medical experts before you make a serious decision that could seriously impact you and your baby.
Necessary C-Sections
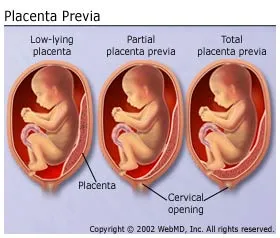
Placenta Previa
Placenta Previa means that your placenta is located above your cervix. Both partial and complete placenta previa (placenta blocks the cervix completely at the time of delivery) is absolutely an indication for c-section. If your placenta blocks your baby’s exit, you are at risk for extreme bleeding, and there is no way for the baby to get out.
What you should know: Placentas can move. Suspected placenta previa can be often be confirmed via ultrasound or even via vaginal exam. Just because you have a low-lying placenta early in your pregnancy does not mean it won’t shift out of the way by the time of delivery. “Marginal” placenta previa, where the placenta is just very close to the cervix, is not generally an indication for c-section. You should know which one you have before you consent; information is power.
Cord Prolapse
If your water breaks, and the cord comes out before the baby, this is Umbilical Cord Prolapse. Cord prolapse is an immediate emergency – either you must immediately deliver vaginally, or proceed directly to the OR. Time is of the essence to save the baby’s life – whichever method gets the baby out fastest should be used.
What you should know: Cord prolapse is much more likely to happen if your baby is premature, and especially if your waters are broken artificially. So, if your care provider offers to "get things moving" by breaking your water with a hook, remember that this is a (small) possibility.
“True” Knot in Umbilical Cord
These are very difficult to diagnose prenatally, but it has happened with 3D ultrasound (which carries risk). A true knot is exactly what it sounds like - it can prevent oxygen from getting to the baby. If one is seen on ultrasound (again, rare – usually they are discovered after delivery), you will likely be sent to the OR.
Placental Abruption
If your placenta detaches from the wall of your uterus while the baby is still inside you, this is a placental abruption. Symptoms are severe abdominal pain, heavy bleeding and back pain. Partial abruption prior to labor is usually treated by bed rest and transfusions, but a complete abruption at any point or any kind of abruption during labor is an emergency situation. Like a cord prolapse, immediate steps need to be taken to get the baby out – immediate vaginal delivery or emergency cesarean.
Click here to read a very sad story about a baby lost due to an abruption - recognizing the symptoms of an abruption and seeking immediate, emergency help is vital to avoiding this tragic result.
Click here to read a very sad story about a baby lost due to an abruption - recognizing the symptoms of an abruption and seeking immediate, emergency help is vital to avoiding this tragic result.
Uterine Rupture
If the uterus tears, an immediate, emergency c-section must be performed to save the life of the mother and baby. This is rare (1/1500 births).
What you should know: Risk of uterine rupture is often given as a reason not to allow VBACs (vaginal birth after cesarean). New research shows that the risk of c-sections may be higher than the risk of rupture, which is very rare.
Toxemia, Severe Pre-Eclampsia, HELLP syndrome, pregnancy-induced hypertension
Pregnancy-induced hypertension is high blood pressure that just keeps rising. Eclampsia, toxemia and HELLP are all potential complications of uncontrolled high blood pressure in a pregnant woman. If PiH isn’t controlled, high blood pressure can cause strokes, cerebral hemorrhage, respiratory distress and even death for the mother, as well as endanger the baby. Toxemia, HELLP and Eclampsia are all potentially deadly complications of uncontrolled PiH.
During pregnancy, there are a number of treatments that can slow disease progression. The only “cure” is delivery. If your blood pressure rises severely enough and quickly enough, it is imperative to get the baby out ASAP. BP over 160/110 is considered severe. Because prolonged labor can be stressful on your body (not that c-sections aren’t!) many doctors prefer to perform a c-section to avoid the possibility of your blood pressure rising further. If the situation becomes unmanageable, immediate action to deliver the baby is required.
You should know: You can reduce the risk of pre-eclampsia with diet and exercise, among other things. Click here for more information about pre-e (to start).
Transverse Lie (baby is lying sideways)
While it is possible to deliver a breech baby vaginally, it is not possible to deliver a baby who is sideways in the womb. That being said, babies move. Just because your baby is sideways NOW doesn’t mean they’ll be sideways when you actually go into labor. 80% of babies who are transverse at 37 weeks have moved when you go into labor! So, don’t just schedule the c-section. Wait to see if baby flips. Check out http://www.spinningbabies.com/ if you want to get your baby on the move.
You should know: While transverse lie is an indication for surgery, breech often isn't. See below.
Acute Fetal Distress
Fetal distress is often used as a reason for c-section delivery, but the definition is nebulous. “We’re worried about the baby” is a sure-fire way to get a laboring woman into the OR without argument. There is a difference between “fetal distress” and “acute fetal distress.” There is a clear definition of acute fetal distress.
Most babies become mildly distressed during labor – so do many moms! Being born is hard work, and it can be stressful. Your baby is often working as hard as you are in this team effort. There’s a BIG difference between being stressed and being in danger. Below are the textbook definitions of “Acute Fetal Distress”. #1, 2 and 5 alone are enough to indicate acute distress. #3 and 4 are used in conjunction with other factors.
1 – Fetal heart rate greater than180 bpm or less than 100 bpm for longer than 4 minutes. Note – an occasional rise or fall to these numbers does not automatically indicate distress. An average over one minute is used.
2- Repeated or variable deceleration. It is normal for the baby’s heart rate to increase and decrease during and after contractions. If the dips become too severe, it can indicate fetal distress. If they don’t happen in time with the contractions (variable), they could be related to something else, such as trouble with the cord or placenta.
3 – Meconium staining of the amniotic fluid. This alone is not necessarily an indication of distress, but it is a symptom. Distressed babies release meconium (poop in the womb). Not all babies who produce meconium in utero are distressed. (Irish girls have pale skin. Not all girls with pale skin are Irish.)
4 – Fetal Movement: frequent decrease and weakening. Again, this is not an indicator by itself; many babies get “quiet” during labor, often just to sleep. If decreased movement happens along with another factor, it’s cause for concern.
5 – Acidosis: If you want to be sure if your baby is in distress and there is time, this is a definitive test. A blood sample is taken from your baby’s head (a tiny scratch). They can immediately test the blood’s PH, oxygen and carbon dioxide levels to see if your baby isn’t getting enough oxygen. This is only possible if the baby’s head is engaged and your water had broken.
pH below 7.20 (Additional information about acidocis here)
pO2 (oxygen level) below 10mmHg
CO2 (carbon dioxide) above 60mmHg
If the baby is in acute distress, it’s time to get the baby out, by the swiftest method possible. Please, if your doctor says the baby is in danger, don't spend time printing out this post and checking the lab work...
More information about fetal distress here
More information about fetal distress here
You should know: If the baby is in mild distress, the first course of action should be to attempt to remove whatever is causing distress. Sometimes, your position can be compressing the cord – occasionally, if you change position (lie on your side, your stomach, or even get in a tub), this can alleviate pressure and allow the cord blood to flow properly. If you’re on pitocin, they should turn it off. Overly strong contractions can stress the baby.
Previous Abdominal Surgery
This is not absolute, but depends on the type of incision and the type of scarring. Certain abdominal surgeries can cause complications during vaginal childbirth. One example is a iliostomy/j-pouch surgery, removal of intestines, vertical previous c-section, or c-section that is not yet healed (less than 1 year). Necessity is dependent on the location of scarring and weaker tissue.
Active Herpes Lesions
If you have genital herpes and have active lesions, you can pass the disease on to your baby at birth. Herpes can be deadly to a newborn, and there is no cure, so they’ve got it for life. Between 10 and 14% of women with genital herpes have a lesion at delivery. The chance of passing the virus to your baby decreases based on the amount of time Mom has had the disease. If you have had herpes for years, the theory goes that you have developed antibodies and will pass these to your baby – even if you have a current lesion. If you acquire herpes during your pregnancy, especially during the 2nd and 3rd trimester, your risk is highest, and you may consider a c-section even if no lesions are present. See this site.
Multiples greater than twins
Triplet and higher deliveries are almost always delivered by c-section. First, these deliveries are rarely full-term, and premature babies may not handle the stress of labor as well as full-term babies. Second, 3+ cords and 3+ placentas can be complicated.
You should know: Twins are regularly delivered vaginally without complication. Even triplets can and have been delivered vaginally (see here for a recent study), but this is rare because triplets and greater so often arrive ahead of schedule.
Known Health Emergency for Baby
If your baby has certain known health issues or birth defects (I hate that phrase, no baby is “defective”) that need to be addressed immediately, a cesarean section may be your best choice. Work with your neonatologist.
Health of the Mother
If a mother is physically incapable of labor because of her own health conditions, c-section is the alternative. Some examples include physical abnormality (certain kinds of dwarfism or pelvic abnormalities), some kinds of paralyzation, out-of-control diabetes, and a few other extreme conditions.
Generally speaking, most women are capable of at least attempting a vaginal birth (there is stress involved in a c-section as well; delivering a baby isn't a walk in the park no matter what your health). You and your doctor need to weigh the benefits and risks.
DEBATED REASONS
These are reasons often given for cesarean sections. There is debate about them. Some people say they’re necessary to mitigate risk, others say that vaginal birth should first be attempted. Do your research, work with your care providers and reach your own conclusions.
If you do decide to have a c-section, armed with the facts, more power to you. My goal is informed consent. If you personally decide that the risks of a c-section are less than the risks of vaginal birth, awesome. I just hate to see women pressured into something they "had" to do when they didn't want it.
Abnormal Fetal Position (breech):
Most midwives and doctors will not deliver a breech baby vaginally – but some will. Many babies are born happily and peacefully in the “frank breech” position, that is, butt first, feet by head. This position is most favorable to vaginal birth, if you can find an experienced provider who is willing to assist. Breech babies have all been delivered successfully vaginally. Breech births do carry higher risks of cord prolapse, increasing with the type of breech delivery. Not included here is Footling breech, which carries the highest risk. In this presentation, baby comes out feet first.
If you attempt vaginal delivery of a breech baby, it is of vital importance that your midwife/OB be well-versed in the intricacies of breech birth. If you can’t find one (providers are much more rare than breech presentations), you may have a c-section. It is important to note that vaginal breech birth should not be attempted without an experienced medical professional who is on board with delivering breech. There are risks to delivering breech vaginally; neonatal death has happened as a result of breach deliveries being handled improperly. Work with your provider to assess your individual situation.
HIV Infection
Some research has shown that HIV transmission from mother to baby can be reduced by surgical delivery. Other research has contradicted this, and found that there is no increased risk with vaginal delivery. For more information, start here and keep on going: http://www.wdxcyber.com/npreg13.htm
Failure to Progress
I would personally argue with this reason. If failure to progress exists but is not accompanied by any health issues for mom or baby (see Acute Fetal Distress above), what most mothers need is patience, not surgery. Mom may need more support. She may need help feeling safe. She may need (eek, omg, yes I’m saying it), help with pain so she can sleep, or other medical assistance. Surgery should be the last option, not the first. Get in a tub. Close the doors and kick the world outside. Listen to soft music, turn down the lights. Magic can happen!
Long ago in caveman days, you wouldn't want to deliver a baby in "unsafe" conditions. Say, there's a warring tribe attacking your cave, or a tiger on the loose - real, physical danger. You wouldn't want to deliver a helpless baby. We're programmed so that labor slows down in periods of stress and fear. Many women who aren't progressing need to feel extra safe and protected before their bodies will allow them to birth their children. Threatening most women with unwanted surgery is not a way to make them feel safe!
Healthy labors can last for days, especially the first time around. This is not necessarily pathogenic. It is annoying to hospital administrations who may want the room for the next woman.... So, personally, unless fetal or maternal health shows signs of deterioration, I'd argue against the knife.
True “failure to progress” is defined as 4 or more hours with no dilation progress, when mom is dilated at least 5cm. Early labor (less than 5cm dilated) can last for a really long time under totally normal circumstances.
Twins (or sometimes even triplets)
Twins are, like breech, a variation on normal. Like breech delivery, you will need to find an experienced caregiver to work with you, but it's absolutely possible. Baby position is also key here - ideal presentation is below, but babies have been successfully delivered in all sorts of presentations.
This is a great site to see videos of twins born vaginally: http://www.givingbirthnaturally.com/natural-childbirth-video.html
This is also a great discussion of mothers who've done it.
An additional complication to the births of multiples is prematurity or babies who are small for their gestational age. Please work closely with a trusted professional to determine your best
An additional complication to the births of multiples is prematurity or babies who are small for their gestational age. Please work closely with a trusted professional to determine your best
 | |
| Twins, both head down, an ideal position for vaginal birth. |
What you should know: Delivering one twin vaginally and then the next by c-section is not unheard of. Some providers (but not all) prefer that you have an OR on "standby" or at least nearby when delivering twins or triplets the old-fashioned way.
Previous Cesarean Delivery
VBACs are not permitted in many hospitals. Why? Well, there have been some studies done that showed an increased risk of uterine rupture in mothers who had previously had a c-section. It scared hospital administrations, and nowadays a lot of hospitals won't let you try vaginally.
The evidence does not support this fear. The risks of a second c-section are usually higher than the risks of attempting vaginal birth. You may have to fight hard for a VBAC, but the evidence is with you.
I am oversimplifying the situations surrounding VBAC - but if you'd like to consider it, please do some research. Not all cesareans are alike, and not everyone is a good candidate for VBAC. If you are a candidate, you may want to consider it. See the bottom of this page for additional information.
I am oversimplifying the situations surrounding VBAC - but if you'd like to consider it, please do some research. Not all cesareans are alike, and not everyone is a good candidate for VBAC. If you are a candidate, you may want to consider it. See the bottom of this page for additional information.
Macrosomia (baby's too big)
This one's tossed around a lot as a reason for surgery. Again, most evidence does not support it.
 |
| I don't remember where I found this picture. |
1 - It is very difficult to truly assess the size of a baby before he's born. Ultrasounds and belly measurements are notorious for being way off.
2 - Most mothers' bodies won't make a baby too big to come out.
3 - Big babies are delivered vaginally all the time. 11-12 pounders!
4 - Baby fat squishes.
If a baby is truly too big to come out the old-fashioned way, that will prove out in labor.
Cephalopelvic disproportion (CPD)
A variation on the "baby's too big" theme, true CPD is also rare, and virtually impossible to diagnose prenatally. CPD means the baby is too large to fit. Sometimes smaller-statured mothers are given this as a reason for c-section.
Tiny mommies have big babies naturally all the time. CPD is real, but it varies widely. Mothers who have had c-sections for CPD have gone on to have successful VBACs.
You should know: If a baby does get "stuck" (shoulder dystocia), changing positions can enlarge the pelvic opening. The Gaskin Manuver is a potentially life-saving technique that can be used in the event of shoulder distocia. The lithotomy position (on your back with your legs up in stirrups) is the one of the *smallest* positions for a woman's pelvis. Flip to all fours or squat, and you can get up to another 3cm in diameter! Shoulder dystocia is a true emergency for the baby, and a competent provider is absolutely essential to saving the baby's life.
Plus-Sized Mama
I am a plus sized mama. I gave birth (vaginally) to a 7 pound baby, who ultrasound "estimated" at 9 pounds 3 days before his birth. Whoops. So much for that "big baby" worry. Some doctors offices will label you "high risk" by the size of clothes you're wearing, and automatically steer your chubby self to the operating table. I call bullsh!t on this one, with some exception.
Generally speaking, if you are healthy enough to vigorously engage in the activity that got you pregnant in the first place, there's no reason that you shouldn't at least attempt a vaginal birth. If, however, you have a hard time getting around, you might have a tough time managing labor. You never know though - you may be surprised with the amazing things your body can do.
In fact, the risks of c-sections are often higher in obese women then the risks of vaginal delivery. Check this out if you're a plus-sized mama-to-be. Personally, I don't see harm in attempting a vaginal birth, no matter what your size - but, again, not a doctor.
You should know: Taking care of yourself during pregnancy and having a supportive care provider are the best ways to ensure a healthy labor and delivery, regardless of your size. If you are plus sized and suspect that your provider is not "size-friendly", switch.
There are undoubtedly many reasons I missed that are either real or dubious reasons for c-section. If you know of any, please comment with them and I will happily edit this article. I will also happily correct any (verifiable) mistakes; I'm not a doctor and I don't play one on the internet.
Ultimately, many c-sections are necessary, but not all of them. Women who have c-sections are no less strong and awesome than those who deliver vaginally, with or without medical assistance. C-sections are not a failure, often they are a massive and amazing miracle that could have resulted in the death of mother or baby not long ago in our history.
What's important through the whole process is informed consent; if you have a c-section, that you understand why it is necessary and agree with your doctors about the choice. Choice, and understanding. C-sections are a blessing and a curse; if used when necessary, c-sections save lives. If unnecessary, they put the health of the mother and baby at increased risk for infection, bleeding, and even death.
What's important through the whole process is informed consent; if you have a c-section, that you understand why it is necessary and agree with your doctors about the choice. Choice, and understanding. C-sections are a blessing and a curse; if used when necessary, c-sections save lives. If unnecessary, they put the health of the mother and baby at increased risk for infection, bleeding, and even death.
Women are people worthy of respect throughout all of labor and delivery. Contrary to media portrayals, we are capable, intelligent and rational people, even after our water breaks. :) We want what is best for our babies, and we want to be treated as adults and active participants in our own healthcare.
Additional Resources:
For more information about the unnecessary c-section epidemic and how it's affecting maternal and neonatal health, check out: http://www.theunnecesarean.com/ and http://www.ican-online.org/
For information about VBACs, click here: http://www.vbac.com/ and http://vbacfacts.com/
For support dealing with birth trauma, including PTSD, visit these sites: http://www.solaceformothers.org/ and http://www.birthtraumaassociation.org.uk/
To learn more about recovering from a c-section, see here: http://www.csectionrecovery.com/ and http://www.csectionguide.com/
Additional Resources:
For more information about the unnecessary c-section epidemic and how it's affecting maternal and neonatal health, check out: http://www.theunnecesarean.com/ and http://www.ican-online.org/
For information about VBACs, click here: http://www.vbac.com/ and http://vbacfacts.com/
For support dealing with birth trauma, including PTSD, visit these sites: http://www.solaceformothers.org/ and http://www.birthtraumaassociation.org.uk/
To learn more about recovering from a c-section, see here: http://www.csectionrecovery.com/ and http://www.csectionguide.com/
Sunday, December 19, 2010
How to Support Breastfeeding without Demonizing Formula
The most positive changes made in the world are not against something but for it.
It can be very tempting to further the normalization of breastfeeding by demonizing formula, or worse, by demonizing formula-feeding mothers. It calls to you. The information's right there, and, if you breastfeed, it makes you feel better about yourself and better about your struggles and your hard work to bring it up. I remember! It's so tempting to respond to the Similac recall with "Serves you right, you should have breastfed" or "Boobs don't have bugs, this is mom's fault." Formula sucks. The educated, informed women who read this stuff already know that. Most of us tried to breastfeed, and we hate that we're giving our babies crap.
Attacking formula-feeding mothers is incredibly detrimental in a number of ways, but the biggest one is that you potentially lose very strong allies by doing so. Me, for example. My nursing in public post has now been read by over 30,000 people in a month (squee!). That's good for breastfeeding. We all need formula-feeding moms on the side of babies and boobs.
Some of the strongest advocates in the intactivist movement are mothers who circumcised their first children. Marilyn Fayre Milos, for example. Some of the strongest advocates for gentle discipline are those who chose corporal punishment first. Some of the strongest proponents of natural birth are those who experienced an over-medicated labor or an "unnecessarian". Many cloth diapering mothers chose cloth because their babies' bottoms reacted badly to disposables.
Many lactivists have never fed their babies an ounce of formula, and some (certainly not all) really seem to enjoy making that fact very known. They should be proud, but sometimes comments cross the line. Formula-feeding mothers are referred to as "lazy", "selfish", "lame", "stupid", "irresponsible" and worse. I'm not pulling this from my own imagination; I am a member of many natural parenting groups and have seen all of these accusations in the last month. I am not an advocate for formula-feeding, any more than I am an advocate for cesareans. I believe that supporting breastfeeding means supporting breastfeeding. No more, and certainly no less.
So, if you want to be a lactivist without pissing off us lazy, irresponsible mothers who didn't try hard enough (ha-ha-ha-ha-ha), what else can you do?
How to Support Breastfeeding
Without Being a Boob
Support nursing in public
I've talked about this one a lot. 'Nuff said.
What you can do: If you are a breastfeeding mother, unashamedly nurse in public. If you can't, thank or at least smile at women who are. Tell the nursing mama that she's welcome to nurse in your living room if she wants to, and she doesn't have to cover up if she doesn't want to. If someone brings up the topic of breastfeeding in public, make your views known, don't stay silent. If you see a nursing mother being asked to leave a public place, come to her aid and fight the flight attendant for her. Support laws that protect nursing mothers.
Support longer, paid maternity leave
Compared to the rest of the developed world, the USA has an embarrassing maternity leave policy. There is no paid maternity leave on a national level. FMLA guarantees 12 weeks of time off every 2 years, without pay, but only if you work for a company with more than 50 employees (in the same state) and have worked there for at least a year. Unpaid. If you work for a small company, just got a new job, or (gasp) have another baby less than 2 years after your last, you're likely out of a job, permanently, if you take leave at all.
Some states extend temporary disability benefits for 6-8 weeks, at a paltry 60% of base earnings, with a low cap. Other states provide nothing. A well-off family can budget for this time, but eventually, the savings run low. A single mother who works at a small company has no real choice - either she goes on welfare or goes back to work. A two-income family, living paycheck-to-paycheck may have no choice at all.
Conversely, Norway and Sweden offer 13-16 months of paid maternity leave at 100% of base earnings. The rest of Europe averages between 16 and 26 weeks (6 months), also paid at 100%. Maternity leave in most of these countries is compulsory - you can't go back to work 3 weeks after your baby is born, even if you "want" to.
There is a direct correlation between the length of maternity leave and breastfeeding success.
- University of California: "A maternity leave of < or =6 weeks or 6 to 12 weeks after delivery was associated, respectively, with a fourfold and twofold higher odds of failure to establish breastfeeding and an increased probability of cessation after successful establishment"
- University of Melbourne: "Mothers who returned to work full-time within three months of birth were twice as likely to have stopped breastfeeding by the time their baby was six months, than those who were not employed. Mothers who returned to work full time between three and six months of birth were three times as likely to have stopped breastfeeding by the time their baby was six months than non-employed women."
When Canada extended maternity leave from 6 months to one year, they saw a large increase in infants who were successfully and exclusively breastfed.
What you can do: Contact your congressional representatives - both senators and representative. Contact your local state representatives and senators. Let them know that you support paid parental leave and extension of FMLA to include all employers and employees, and to extend to at least 52 weeks.
Support certified lactation consultants
Poor medical advice for breastfeeding is pervasive through the system. Certified lactation consultants can save a breastfeeding relationship. Unfortunately, they are expensive to hire, and their services are not usually covered by medical insurance.
A lactation consultant can take a mother from the brink of quitting to a healthy, happy nursing relationship. She can save damaged, bleeding, painful nipples. She can fix bad latches and bad positioning, she can un-advise against bad advice. She can make magic happen - if she is given the opportunity.
The average visit to a lactation consultant costs $250-$300 - and while it's certainly cheaper than a year's worth of formula, to the low-income mother on unpaid maternity leave, it might as well be a million bucks. After all, formula is covered by WIC. LCs are a luxury that many women cannot afford.
Further, they're not that easy to find. Sure, if you're part of the AP community, you know the names of a few off the top of your head - but where would the average mother get this information? I hadn't heard of lactation consultants until I started to really research...and not all mothers research.
What you can do: Call your insurance company and ask if they cover lactation consultants. If they don't, ask why not, and ask how you can complain in writing. Make sure your pregnant friends know the names of LCs in their area. Provide a list of LCs to your local hospitals, visiting nurses associations, YMCAs and OB offices. Post the date and times of local LLL meetings on community bulletin boards and in supermarkets. Provide that information to teen mother support groups. If you are a LC, consider donating some of your time or offering low-cost services, even on a group basis to low-income mothers.
Support gentle birth
Getting a good start at breastfeeding is so very important. Maternity leave, lactation consultants, and pediatrician support only work if a mother begins her breastfeeding relationship right. Baby-friendly hospitals are a start. Baby-friendly hospitals aim to have a 100% breastfeeding rate, and they educate staff appropriately.
| 1 - | Have a written breastfeeding policy that is routinely communicated to all health care staff. |
| 2 - | Train all health care staff in skills necessary to implement this policy. |
| 3 - | Inform all pregnant women about the benefits and management of breastfeeding. |
| 4 - | Help mothers initiate breastfeeding within one hour of birth. |
| 5 - | Show mothers how to breastfeed and how to maintain lactation, even if they are separated from their infants. |
| 6 - | Give newborn infants no food or drink other than breast milk, unless medically indicated. |
| 7 - | Practice “rooming in”-- allow mothers and infants to remain together 24 hours a day. |
| 8 - | Encourage breastfeeding on demand. |
| 9 - | Give no pacifiers or artificial nipples to breastfeeding infants. |
| 10 - | Foster the establishment of breastfeeding support groups and refer mothers to them on discharge from the hospital or clinic |
I'm going to add on steps 11-20:
| 11 - | Limit interventions in labor to those that are truly medically necessary for the health of mother and baby. |
| 12 - | Do not circumcise baby boys or girls for non-medical reasons. |
| 13 - | Encourage mothers and babies to attempt the "breast crawl" after delivery. |
| 14 - | Teach baby-wearing |
| 15 - | Provide safe co-sleeping guidelines |
| 16 - | Arrange for lactation consultant follow-up home visits after discharge. |
| 17 - | Provide midwifery care for lower risk births. |
| 18 - | Provide prescriptions for breast pumps to be covered as durable medical equipment by insurance |
| 19 - | Encourage immediate and prolonged skin-to-skin contact, as well as a gentle post-birth environment. |
| 20 - | Skip the hospital If you are low-risk, try to give birth at home. |
What you can do: If you gave birth naturally or gently, tell your birth story. Support home birth. Support midwifery. Contact your local hospital and ask if they have been certified "baby-friendly" by the WHO. If not, ask why not. Drop off breastfeeding information at your local maternity ward and at your OB's office. Support the right to genital integrity and openly oppose routine infant circumcision.
Support the re-education of medical professionals
The worst breastfeeding advice I have ever heard came out of the mouths of medical professionals.
- "Only feed for 10 minutes on each side, any more is unnecessary."
- "Only nurse every 3-4 hours, any more and he's using you as a pacifier."
- "We have to give her formula until your milk comes in."
- "You can't have a glass of wine if you're nursing."
- "Pregnant women's milk is not good for older babies. You need to wean."
- "After 6 months, there is no nutritional value to mother's milk; it's just for comfort."
- "One bottle of formula won't hurt anything."
- "Breast milk doesn't have enough vitamins. You need to give your baby vitamins unless you formula-feed."
- "You can't breastfeed if you take_____ medicine" (without checking if it is actually true)
- "Your baby isn't growing fast enough. You need to supplement with formula."
Sometimes, there is a real, medical reason to stop breastfeeding or supplement with formula. That is rare - but the majority of women trust their doctor over their own gut feeling or their own research. Medical professionals need to be educated on the facts. More breastfeeding relationships have been ruined by pediatricians, nurses and obstetricians than all the free cans of formula in the world. One bottle of formula *does* harm a nursing relationship. Nursing on-demand really means on demand! It is so hard to question your child's doctors.
Every new breastfeeding mother I know has worried, "how do I know my baby is getting enough food?" especially because all newborns seem hungry all the time. One statement from a doctor about low percentiles or supplementation can be the beginning of the end of a healthy relationship. Doctors need to be educated about alternative ways to increase supply if there really is a problem - and need to realize that formula should be the last resort, not the first reaction.
What you can do: Talk to your pediatrician about breastfeeding. Invite local pediatricians to attend LLL meetings. Encourage your local hospital to adopt baby-friendly policies. Make sure every pregnant woman knows how to find accurate information. Bookmark KellyMom.com on her computer. While you're at it, send the link to your pediatrician. Write to the AAP whenever you hear a doctor saying something untrue about breastfeeding, to encourage further training.
Support nursing rooms in workplaces, schools, and public buildings
 |
| Nursing rooms are common in Malaysia. |
Not all women are comfortable nursing in public. Nursing rooms are a wonderful amenity that should be as available as bathrooms. Many laws (but not all states) require that nursing mothers be provided a clean, safe and comfortable place to pump in the workplace....but this is rarely true. Most moms end up pumping in bathrooms, spare conference rooms, supply closets or cars.
Schools are especially key - not just for the teachers, but also for the students. Breastfeeding rates among teen mothers are appalling. Not all mothers are happily married stay-at-home mommies.... in fact, most aren't. Supporting nursing and pumping means supporting it in high schools, Walmart break rooms, and your local fast food joint.
What you can do: If you work, ask your HR department about space for nursing mothers. Contact your local high school and encourage the school to set aside a room for mothers to pump or nurse. Ask at your local government building.
Support breast milk donation
There are real, undeniable, and unavoidable reasons that breastfeeding may not be possible, including but not limited to:
- Death or incapacity of the mother
- Inability of the mother to produce sufficient milk, due to PCOS, insufficient glandular tissue, mastectomy, etc.
- Adoption of a child (before re-lactation or if it is not possible)
- Medical conditions that require unsafe medication to manage

Babies should be able to drink human milk, even if their mothers can't provide that milk to them.
Unfortunately, "official" milk banks are extremely selective and extremely expensive. I contacted two when I had to stop breastfeeding, and I was told that milk was reserved for sick babies, and that even if they had some, the price for the milk was $3.50 an ounce and not covered by insurance. For a baby who eats 32 ounces a day, that is simply impossible - and we are a well-off family.
Between then and now, a new organization has come onto the forefront, Eats on Feets, which will connect nursing mothers with women like me, who need donated milk for our babies. It's still in its infancy, and private milk donation has a long way to go toward being socially acceptable again, but it is a place to begin. Right now, there is less milk than women who need it.
What you can do: Donate any extra milk you have. Support Eats on Feets. Talk about breast milk donation, and challenge gut reactions that it's "icky." If your local EoF is active and has milk available, reach out and let folks know it's there for the taking.
Support media exposure of breastfeeding
1977, Buffy explains breastfeeding to Big Bird.
Bottles are everywhere. Every time you see a baby on TV, you see a bottle. Children's cartoons are filled with bottles, but nursing is taboo. This is an echo on nursing in public, and all the same reasons apply. Normalizing breastfeeding means that it has to make its way onto television.
What you can do: Contact PBS and ask them to run another special on television. Every time you see a baby bottle on TV, comment online at the station and on facebook/twitter. If you do see nursing on TV, send a compliment (I sent one to the director of "Four Christmases", which was the first movie I've ever seen with casual nursing and lots of breastfeeding mentions without being a movie about babies)
Oppose Unethical Marketing of Formula
Haha, exception proves the rule, right?
Yes, the whole point of this article is not to demonize formula or formula-feeding moms. Demonize the mainstream formula companies as much as you want. Go for it. Thanks to these jerks, babies all over the world die, and I fed my kid bugs, while they profit massively.
Formula companies advertise *everywhere*. Boobs don't get glossy ads in Parents' magazine. Formula companies are regulated in what they can say, but boy, do they squeeze close to that edge! "Closer than ever to breast milk" is such a misleading statement. I can make Coca-Cola "closer" to breast milk by adding DHA and probiotics. It doesn't make it close. Obviously, Similac is a better choice for your baby than Coke. BUT, the difference between formula and breast milk is as far the difference between formula and soda.
Especially abhorrant are the advertisements in developing countries, where a lack of access to clean drinking water makes formula truly life-threatening. If you don't have clean water, breast milk is vital to the survival of babies, yet companies like Nestle see opportunities for "new marketshare" and plaster with this messaging.
Even the "Breast is Best" campaign is tainted by formula marketing. It insinuates that perfect moms breastfeed, but who's perfect anyway? Breast isn't just best - it's NORMAL. It's what babies should eat, absent extenuating circumstances. Ads plastered on TV, in magazines, in doctors' offices and in hospitals make formula seem like the normal choice. Breast milk isn't a "nice option" like organic foods or designer baby clothes. It's necessary, normal, and appropriate. It's how babies were made to be fed. It's how moms were made.
What you can do: Boycott Nestle. If you subscribe to any magazines that advertise formula, write to them and ask for "fair and balanced" advertising that encourages a one-to-one ratio of breastfeeding and formula references in their publication - or better yet, ask that they not advertise formula at all. If you see coupons or advertising at your doctors' office, ask your doctor why they are advertising formula.
So, are you ready? This is the harder road, but it's the one that makes a difference. Invite your formula-feeding friends (if you have any) to join you in a fight for mothers' and babies' rights. There's a lot of us, and we can actually make something happen....if we don't spend our time pointing at each other.
Thursday, December 16, 2010
My Baby Boy and Me
I didn't write this. I did, however, print it and have it folded by my son's rocking recliner (forget the rocking chair!). When it's 4am and I've been up 3 times already, I read it. This time is so precious, and so fleeting.
My Baby Boy and Me
It's 3am, they're all asleep and no one's here to see
As we rock slowly back and forth, My Baby Boy and Me.
His little head is feather light tucked up against my chin
I hold his tiny hand in mine and stroke his baby skin.
The house about us creaks and groans the clock hands creep around
He snuggles closer to me still and makes his baby sounds.
I love these quiet hours so much and cherish every one
store memories up inside my heart for lonely nights to come.
All too soon he'll be grown up, his need for Mommy gone
but until then I still have time for kisses and for song.
Time for quiet hours like this with him cuddled in my arms
where I wish he'd always stay protected safe and warm.
And yet I know the day will come when his tiny little hand
will be much bigger than my own he'll grow to be a man.
But until then he's mine to love with no one here to see
as we rock slowly back and forth My Baby Boy and Me.
by Dusty Fulbright
Labels:
attachment parenting,
bedsharing,
cosleeping,
Poetry
Tuesday, December 14, 2010
Birth Plans and Birth Realities
I'm was going to get my whole "birth story" up on here some day (my son's now 9 months old, hmmmm). Meanwhile, however, I was digging through some old files and I found my Birth Plan, and thought this might be a good way to tell it!
I gave birth to David #9 at the birth center of a small community hospital, about an hour from my home. I picked the hospital very much on purpose - they are the only one in the state that allows water births, they don't have a nursery, they're "baby-friendly", and I absolutely loved my midwife. I wrote up a plan, and not everything went according to plan.
Overall, I would give my birth experience an 8/10 (the baby gets 11 out of 10, I'm talking about the experience). I've heard the question asked often - "Does anyone have a birth plan for people who want to birth naturally in the hospital?" I do....but it's only a plan. If you want to be guaranteed the best shot at a natural birth, stay home. If, however, you do choose to have a hospital birth, I found this plan to be a pretty good one.
Anyway, without further ado, here's the plan, and how it actually turned out.
Arrival Plan
• Can I have the room with the tub? Pretty please?
• Please assign a nurse who doesn’t think I’m insane for wanting a med-free birth
• No IV, hep lock if necessary
• Let Me Eat and Drink (and puke…yeah, I expect it)
• I’d like to wear my own clothes
• Intermittent monitoring (via Doppler if possible, please don’t strap me in bed)
What actually happened:
My first sign of labor was my water breaking all over the bed at home at 37 weeks on the dot. We drove to the hospital, and I got the room with the tub, but never ended up using it. I was assigned a nurse who didn't think I was nuts. A saline lock was started 3 hours after I arrived - this was not a big deal. IV wasn't started until later. I was allowed to eat and drink whatever I wanted. I wore my own clothes for 14 hours, until the plan went off track. Intermittent monitoring was also permitted until pitocin was administered; after that it was continuous.
Labor Plan:
I would prefer to avoid interventions, but we trust your medical opinion of what may be necessary. Please discuss any interventions you believe may be necessary with me and my husband.
• I’m using hypnosis; please don’t try to talk to me during contractions (pressure waves). Dave or Mom can talk for me if it’s an emergency.
• In hypnosis I am very susceptible to suggestion. Please be careful with what you say – avoid words like “pain” and use “pressure”.
• Ahhh! Bright Light! I’d like to keep the lights low, if possible.
• Play that funky music…. I’m bringing my iPod and speakers.
• I know what my pain relief options are. I’ll ask for drugs if I want them. Promise.
• Limit the number of internals, and don’t tell me how far I am dilated unless I ask.
• I would like to birth my baby in the water.
• If I can’t be in the tub, please let me choose the position that is most comfortable for me.
• I would like to try “mother-directed pushing” rather than counting to 10.
• Please let me know how I may reduce tearing.
• I would prefer to tear rather than have an episiotomy.
What Actually Happened:
For the first 14 hours, I got everything I asked for. We had a lovely playlist (5 hours long) going on the iPod, the lights were dim, nobody asked me if I wanted drugs, I was given a ball to bounce on, a bar to hold, and given free range of the hospital to walk. My progress wasn't checked (although they did ask).
After 14 hours, I consented to be checked, thinking I would be 7-8cm....but I was 3cm dilated. My midwife was concerned about infection, given the extended length of time since my water had broken. She recommended that I be given pitocin - which meant that I was stuck in bed with a monitor on, and that water birth was no longer an option. After an hour with pitocin, I gave in to the epidural. The contractions had quickly gone from something I could handle to absolutely miserable, especially since I no longer had the ability to move around. My "unmedicated" birth was gone, I couldn't use the tub, and in many ways my will was broken. I know there are moms who can do pitocin without an epidural...I am not one of them.
I will probably always wonder if Pitocin was truly necessary. In retrospect, I should have asked to use the tub to see if that would help me progress....but when your contractions are 2 minutes apart and you haven't slept in 24 hours, you don't see clearly. Ultimately, I trusted Kathy - she was the expert, and I trusted her professional opinion and her 20+ years of midwifery, including her own 5 natural births....but still, I question.
When, eventually, I got to 8cm, my midwife turned the pitocin and the epidural off. I love her for that! She told me - and the nursing staff - not to push unless I had absolutely no choice, until my body told me "push or die!" The epidural wore off just as that feeling hit me. Well, first I threw up all over my husband, then I had to push like it was the end of the world.
Just as the last of the epidural wore off, I had full feeling in my body and I was able to first sit up during contractions, then squat on the floor, holding the bed. For the first 40 minutes, all pushing was "mother-directed." I started to give up a little (it had been 28 hours), and Kathy did have me do 3 massive "count to ten" pushes until she saw David begin to crown.
Then, she had me stop pushing. Hardest thing I've ever done! She had me stop pushing and hold, to let my body stretch. She instructed me to give tiny pushes even though I wanted to give it everything - and David gently wiggled out of me. I actually had an orgasm. Seriously. I laughed out loud, and it was the best feeling ever. Ten minutes after I gave birth, I asked my husband when we could do it again.
The music was still playing, the lights were still low, and Kathy was wearing cowboy boots and jeans. No scary medical equipment, no shouting - peaceful and lovely, just how I had envisioned it. "I Just Haven't Met You Yet" played when David was born, and Rascal Flats "God Bless the Broken Road" was playing when I first held him. I'll never forget that!
I didn't tear or need an episiotomy. YAY for stretchy lady-bits! Oh, and because I know I was concerned, especially with the Ulcerative Colitis....I didn't poop on my midwife. Heh.
When the Baby is Born
If mom and baby are healthy….
• I would prefer that the baby be placed on my stomach immediately for skin-to-skin contact for at least 1 hour after birth.
• I would like cord clamping to be delayed at least 5 minutes or until the cord stops pulsing.
• I would like to deliver the placenta without pitocin or traction.
• If I need stitches, please provide anesthetic (local or otherwise).
• I would like to delay all newborn procedures – including weight and length checks- until after we have had the opportunity to breastfeed.
• I would like to allow the “breast crawl” if possible.
• Please don’t allow any visitors in until we say we’re ready for them.
• We plan to exclusively breastfeed. Please do not offer pacifiers or formula.
• Our pediatrician will handle the HepB vaccine; please do not administer.
• Can we use liquid vitamin K instead of the injection?
• Eye goop (antibiotics) should be delayed until after the first breastfeeding session.
• Do not circumcise, and do not retract. (Click here for the 50 reasons we didn't)
• The baby should be with Mom or Dad at all times for any procedure (including first bath).
What actually happened
David came out a little blue, so Kathy delayed clamping and held him below me until he pinked up - no suctioning or toweling. I'm convinced that delayed cord clamping saved him a trip to the NICU. He was placed on my stomach, and did the Breast Crawl and self-latched. It was the most amazing thing I have ever seen. We were allowed 30 minutes of uninterrupted bonding/breastfeeding time, before any weighing or cleaning was done.
It would have been longer than 30 minutes...but my placenta wasn't moving. At 30 minutes, the nurses started to massage my stomach (OW), no dice. At 40 minutes, they started pitocin again....I disliked it as much the second time around! At 55 minutes, I started to bleed heavily and they called to prep the OR. At the very last minute, Kathy's partner and ex-husband Doug-the-OB asked me if I wanted him to try a manual removal, rather than a D and C.
I didn't want to be separated from my baby and I didn't want to go under ansethesia, so I said yes. They cleared the room, my mom and husband were actually escorted out of the maternity ward. Kathy held my shoulders, and Doug reached up inside me and manually removed my placenta. My poor husband said he could hear me screaming from across the hospital. Hurt like hell....but given the choice, I would probably do it again to avoid the operating room.
In the 24 hours that followed (we were released early by request, I felt great), there was never a mention of formula or pacifiers. We were visited by 3 lactation consultants! There was no question about the Hep B vaccine, and liquid vitamin K was supplied. No eye goop either, and no pressure to use it. They did ask us 4 times if we wanted to have David circumcised - but when we said no, our decision was met with relief and respect, depending on who asked.
David was only away from my side for 10 minutes, held lovingly by his midwife while I showered and my husband was on his way back to the hospital with the carseat.
Summary
Overall, I believe my hospital experience was far superior to what many mainstream hospitals will offer a laboring woman. I was respected, my wishes were respected, and the hospital waited longer than most would to intervene - 14 hours after my waters released, and almost an hour on a retained placenta. I have since learned that most hospitals will only allow 4-6 hours of "no progress" and a hard rule of 30 minutes for placental expulsion.
Also, even though not everything went according to "plan", we were still able to get back on track. I had an orgasmic, medicated birth. I've still never heard of another. I thought it was all or nothing, and again the world showed me another shade of gray! Next time around, I'd like to have a home birth, but I'm not unhappy with the experience I had.
So, if you choose a hospital birth and things don't go as planned, don't give up on the whole thing! You can have a beautiful, amazing, mind-blowing experience in spite of it all. And, at the end of it all, I got to bring home the best (early) birthday present ever, blue eyes and all.
I gave birth to David #9 at the birth center of a small community hospital, about an hour from my home. I picked the hospital very much on purpose - they are the only one in the state that allows water births, they don't have a nursery, they're "baby-friendly", and I absolutely loved my midwife. I wrote up a plan, and not everything went according to plan.
Overall, I would give my birth experience an 8/10 (the baby gets 11 out of 10, I'm talking about the experience). I've heard the question asked often - "Does anyone have a birth plan for people who want to birth naturally in the hospital?" I do....but it's only a plan. If you want to be guaranteed the best shot at a natural birth, stay home. If, however, you do choose to have a hospital birth, I found this plan to be a pretty good one.
Anyway, without further ado, here's the plan, and how it actually turned out.
The view from the birthing center at Newport Hospital.
Not taken by me, but I remember vividly being in labor and watching the sun rise like this over the bridge during a contraction.
Arrival Plan
• Can I have the room with the tub? Pretty please?
• Please assign a nurse who doesn’t think I’m insane for wanting a med-free birth
• No IV, hep lock if necessary
• Let Me Eat and Drink (and puke…yeah, I expect it)
• I’d like to wear my own clothes
• Intermittent monitoring (via Doppler if possible, please don’t strap me in bed)
What actually happened:
My first sign of labor was my water breaking all over the bed at home at 37 weeks on the dot. We drove to the hospital, and I got the room with the tub, but never ended up using it. I was assigned a nurse who didn't think I was nuts. A saline lock was started 3 hours after I arrived - this was not a big deal. IV wasn't started until later. I was allowed to eat and drink whatever I wanted. I wore my own clothes for 14 hours, until the plan went off track. Intermittent monitoring was also permitted until pitocin was administered; after that it was continuous.
Labor Plan:
I would prefer to avoid interventions, but we trust your medical opinion of what may be necessary. Please discuss any interventions you believe may be necessary with me and my husband.
• I’m using hypnosis; please don’t try to talk to me during contractions (pressure waves). Dave or Mom can talk for me if it’s an emergency.
• In hypnosis I am very susceptible to suggestion. Please be careful with what you say – avoid words like “pain” and use “pressure”.
• Ahhh! Bright Light! I’d like to keep the lights low, if possible.
• Play that funky music…. I’m bringing my iPod and speakers.
• I know what my pain relief options are. I’ll ask for drugs if I want them. Promise.
• Limit the number of internals, and don’t tell me how far I am dilated unless I ask.
• I would like to birth my baby in the water.
• If I can’t be in the tub, please let me choose the position that is most comfortable for me.
• I would like to try “mother-directed pushing” rather than counting to 10.
• Please let me know how I may reduce tearing.
• I would prefer to tear rather than have an episiotomy.
What Actually Happened:
For the first 14 hours, I got everything I asked for. We had a lovely playlist (5 hours long) going on the iPod, the lights were dim, nobody asked me if I wanted drugs, I was given a ball to bounce on, a bar to hold, and given free range of the hospital to walk. My progress wasn't checked (although they did ask).
After 14 hours, I consented to be checked, thinking I would be 7-8cm....but I was 3cm dilated. My midwife was concerned about infection, given the extended length of time since my water had broken. She recommended that I be given pitocin - which meant that I was stuck in bed with a monitor on, and that water birth was no longer an option. After an hour with pitocin, I gave in to the epidural. The contractions had quickly gone from something I could handle to absolutely miserable, especially since I no longer had the ability to move around. My "unmedicated" birth was gone, I couldn't use the tub, and in many ways my will was broken. I know there are moms who can do pitocin without an epidural...I am not one of them.
I will probably always wonder if Pitocin was truly necessary. In retrospect, I should have asked to use the tub to see if that would help me progress....but when your contractions are 2 minutes apart and you haven't slept in 24 hours, you don't see clearly. Ultimately, I trusted Kathy - she was the expert, and I trusted her professional opinion and her 20+ years of midwifery, including her own 5 natural births....but still, I question.
When, eventually, I got to 8cm, my midwife turned the pitocin and the epidural off. I love her for that! She told me - and the nursing staff - not to push unless I had absolutely no choice, until my body told me "push or die!" The epidural wore off just as that feeling hit me. Well, first I threw up all over my husband, then I had to push like it was the end of the world.
Just as the last of the epidural wore off, I had full feeling in my body and I was able to first sit up during contractions, then squat on the floor, holding the bed. For the first 40 minutes, all pushing was "mother-directed." I started to give up a little (it had been 28 hours), and Kathy did have me do 3 massive "count to ten" pushes until she saw David begin to crown.
Then, she had me stop pushing. Hardest thing I've ever done! She had me stop pushing and hold, to let my body stretch. She instructed me to give tiny pushes even though I wanted to give it everything - and David gently wiggled out of me. I actually had an orgasm. Seriously. I laughed out loud, and it was the best feeling ever. Ten minutes after I gave birth, I asked my husband when we could do it again.
The music was still playing, the lights were still low, and Kathy was wearing cowboy boots and jeans. No scary medical equipment, no shouting - peaceful and lovely, just how I had envisioned it. "I Just Haven't Met You Yet" played when David was born, and Rascal Flats "God Bless the Broken Road" was playing when I first held him. I'll never forget that!
I didn't tear or need an episiotomy. YAY for stretchy lady-bits! Oh, and because I know I was concerned, especially with the Ulcerative Colitis....I didn't poop on my midwife. Heh.
David James IX, 7lbs even.
When the Baby is Born
If mom and baby are healthy….
• I would prefer that the baby be placed on my stomach immediately for skin-to-skin contact for at least 1 hour after birth.
• I would like cord clamping to be delayed at least 5 minutes or until the cord stops pulsing.
• I would like to deliver the placenta without pitocin or traction.
• If I need stitches, please provide anesthetic (local or otherwise).
• I would like to delay all newborn procedures – including weight and length checks- until after we have had the opportunity to breastfeed.
• I would like to allow the “breast crawl” if possible.
• Please don’t allow any visitors in until we say we’re ready for them.
• We plan to exclusively breastfeed. Please do not offer pacifiers or formula.
• Our pediatrician will handle the HepB vaccine; please do not administer.
• Can we use liquid vitamin K instead of the injection?
• Eye goop (antibiotics) should be delayed until after the first breastfeeding session.
• Do not circumcise, and do not retract. (Click here for the 50 reasons we didn't)
• The baby should be with Mom or Dad at all times for any procedure (including first bath).
What actually happened
David came out a little blue, so Kathy delayed clamping and held him below me until he pinked up - no suctioning or toweling. I'm convinced that delayed cord clamping saved him a trip to the NICU. He was placed on my stomach, and did the Breast Crawl and self-latched. It was the most amazing thing I have ever seen. We were allowed 30 minutes of uninterrupted bonding/breastfeeding time, before any weighing or cleaning was done.
It would have been longer than 30 minutes...but my placenta wasn't moving. At 30 minutes, the nurses started to massage my stomach (OW), no dice. At 40 minutes, they started pitocin again....I disliked it as much the second time around! At 55 minutes, I started to bleed heavily and they called to prep the OR. At the very last minute, Kathy's partner and ex-husband Doug-the-OB asked me if I wanted him to try a manual removal, rather than a D and C.
I didn't want to be separated from my baby and I didn't want to go under ansethesia, so I said yes. They cleared the room, my mom and husband were actually escorted out of the maternity ward. Kathy held my shoulders, and Doug reached up inside me and manually removed my placenta. My poor husband said he could hear me screaming from across the hospital. Hurt like hell....but given the choice, I would probably do it again to avoid the operating room.
Wow, that's a terrible picture...but a beautiful baby!!
In the 24 hours that followed (we were released early by request, I felt great), there was never a mention of formula or pacifiers. We were visited by 3 lactation consultants! There was no question about the Hep B vaccine, and liquid vitamin K was supplied. No eye goop either, and no pressure to use it. They did ask us 4 times if we wanted to have David circumcised - but when we said no, our decision was met with relief and respect, depending on who asked.
David was only away from my side for 10 minutes, held lovingly by his midwife while I showered and my husband was on his way back to the hospital with the carseat.
Summary
Overall, I believe my hospital experience was far superior to what many mainstream hospitals will offer a laboring woman. I was respected, my wishes were respected, and the hospital waited longer than most would to intervene - 14 hours after my waters released, and almost an hour on a retained placenta. I have since learned that most hospitals will only allow 4-6 hours of "no progress" and a hard rule of 30 minutes for placental expulsion.
Also, even though not everything went according to "plan", we were still able to get back on track. I had an orgasmic, medicated birth. I've still never heard of another. I thought it was all or nothing, and again the world showed me another shade of gray! Next time around, I'd like to have a home birth, but I'm not unhappy with the experience I had.
So, if you choose a hospital birth and things don't go as planned, don't give up on the whole thing! You can have a beautiful, amazing, mind-blowing experience in spite of it all. And, at the end of it all, I got to bring home the best (early) birthday present ever, blue eyes and all.
Subscribe to:
Comments (Atom)